This "blog" has been dormant for 5 years because lol, who writes blogs anymore. But with the 5th anniversary of the Covid-19 outbreak landing in the US, I've been reflecting on the things I've lost over 5 years.
Public Health Stories from a Super Legit Expert
...in training
Saturday, April 5, 2025
What Five Years Took
Revenge of the Nerds
I've always been friends with the conscientious, smart kids. In my senior year in high school, my friends and I took out our planners so we could coordinate a skip day that didn't conflict with a test in any of our classes. Today's run up to the Stand Up for Science rally feels a lot like that again. Calendars have been cleared. Signal groups created. And the government employees have taken time off so as not to violate the Hatch Act. I don't know what the turnout will be. And I certainly don't know what will happen beyond today. But the nerds are so angry. And want to feel like we are doing something to stop the avalanche. I lose my words whenever I get to this point, when I want to insert a sentence about what the indiscriminate cuts have meant. They've been so wide ranging and random. It's hurt me, but you as well-- whether that's through fewer spots for grad students, lapses in food safety, or monitoring the weather we all experience. In the midst of all the impact big and small, to pick something specific, I am going today because I care deeply about the health and healthcare experiences of veterans.
Friday, March 27, 2020
Everyone's a Cynic
Within weeks of working my first job out of Bowdoin College and foray into the world of academic research, I learned that my suspicions of the world were true. Poring through whistleblower affidavits, I saw how Big Pharma was as aggressive as I’d imagined. The Food & Drug Administration was funded by the same drug manufacturers it was commissioned to monitor. The game was rigged. Yet cynicism was not the transformative lesson of my early career. It was how the researchers I worked with dealt with their knowledge of an imperfect system. Even as they kept a critical eye on them, they cooperated with pharmaceutical companies and government agencies to produce research that evaluated the impact of flawed policies. Cynicism could not deter them from changing the world. And I want to change the world through health services research.The essay itself wasn't that great. It may be the reason I didn’t get into some schools (that one school, in Boston). But I’ve been thinking a lot about cynicism and the rigged game lately. More so than usual. Mostly though, I have been so very angry, disappointed, and anxious. These emotions are not new to me (however suave I may seem to you). They are par for the course in public health, in healthcare, and in health policy. We study bad outcomes and how to prevent them. We yell into voids and shake our fists government inaction (see also, Affordable Care Act; see also, gun violence). We even shoulder some of the blame. If only we were better communicators, maybe they would've listened.
Yet cynicism was not the transformative lesson of my early career. It’s the belief that we can change the broken world. I have so many friends and colleagues in this fight. I look to those who rail back against the incompetence and demand better. Who speak plain truths to the public even when they are harassed for doing so. I look to those who are building models and creating the evidence base for how we should move forward. I look to the healthcare workers who have prepared their wills, and who volunteer to go into the hospital knowing full well how unprepared they are. I look to you. You who are still reading and playing along by staying home. By helping your neighbors. By sharing laughter and good information. And we do it regardless of who is in office, or how smoothly our systems work. We do it because we can change the world (see also: history of hand washing).
Thursday, March 19, 2020
How Long Must This Go On?
Where Are You Getting Your Information?
https://www.statnews.com/tag/coronavirus/ has good, no-frills science reporting.
What Do I Do If I Get Sick?
As with anything else I write-- I am not a medical doctor. I am just offering general guidelines. For specific treatment decisions about your own health, talk to your doctor (if you don't have one, times like these are why they're helpful. Here's an old blog post about searching for doctors).
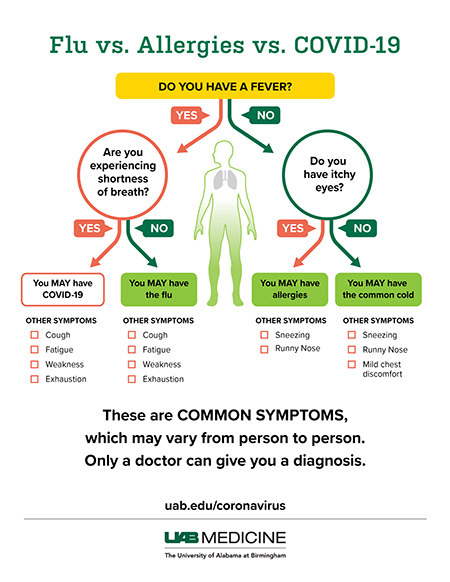
First off, a couple of handy charts to tease out some common symptoms. Everyone is different, but in general, these are the symptoms that help distinguish one from the other.
There are actually several good sources out there that answer this question. The CDC is one. What I write below is basically a wordier version of what they say. Because I'm not as good as editing.
Now, if you feel like you don't have Covid-19 and your health issue is something that can be managed with rest, fluids, and over the counter meds, and if you feel 0-4 on a scale of 0 to terrible, then you should do just that. Rest. Fluids. Over the counter meds to manage symptoms as needed. The end. Also, stay the fuck home.
If you think you have Covid-19 or if you feel terrible (5 or above on the scale) for other reasons, it's time to call up your doctor. Do NOT go to the emergency room. Do NOT show up to urgent care clinics. Doing either will add burden to an overwhelmed system and put you at more of a risk of contracting Covid-19. Most doctor's offices have shifted to phone calls or video visits in recent days. There are lots of "patient portals" and things you may be asked to sign up for to facilitate this process. Some might include screening questions (for Covid-19) to help you decide if and when you should call for help. You can find all those things by calling up your doctor or going directly to their clinic website if they have one. If you're already enrolled in a portal, you can schedule a visit without talking to anyone. Here's an example of one, from a health system in Michigan.
If your symptoms match with those of Covid-19 but they are not severe, you will likely not be tested. Although testing is becoming more available, many areas of the country are still behind. Testing requires a lot of resources beyond the tests, like time, personnel, and protective equipment. Unfortunately, an overwhelmed system does not have enough of any of those to spare. It's unfair. But it's American in 2020. So even if you have Covid-19, you may not be tested. Stay home. Isolate yourself from everyone, including those you live with, until you get better (better = until you have x number of symptom free days). If your conditions change according to your assessment, contact your doctor immediately. It's important for people with mild cases of Covid-19 to not just stay home but also isolate from everyone, including those in your household, because, I don't know if you know this, but Covid-19 is a novel disease. It's highly contagious. Not infecting other people means lowering the number of cases that may stress the health system.
(What if you don't have a doctor? That gets a little harder. If you have health insurance, I'd find a primary care practice that can take you. Or call an urgent care clinic that you have access to. Whatever you do, do not show up to the emergency room unless you're actively dying. Always call ahead.)
